BOSTON — Tony McKoy, Jr. was ready to eat. Black chef’s hat on his head, apron tied on, the 5-year-old contemplated his favorite foods, prompted by his mother, Shaquana Peebles.
“Pineapple!” he said, savoring its sweetness with his eyes closed while he imagined biting into one. Also, brownies made with black beans. PB&J. Spaghetti.
Tony’s enthusiasm for food is a remarkable turnaround for a child who wasn’t growing as well as he should just a couple of years ago.
“I really did not think that his pickiness would turn and involve wanting to be a chef and to learn about food and everything. It shocked me completely,” Peebles said as she held Tony’s one-month-old brother, Egypt, to her chest. “I’m making spinach, and he says, ‘Oh, this is so good.’ And I’m like, ‘Who are you?’”
Tony’s pediatrician had recommended that they attend the GROW Clinic for Children at Boston Medical Center, which in addition to providing medical services for children diagnosed with failure to thrive, helps people eat and cook more nutritious meals through its Teaching Kitchen initiative. Participants gather in a glass-walled partition off the hospital cafeteria for over 25 classes a month, which range from medically tailored programs for specific patient groups to educating Boston Medical Center staff to support their own wellness.
Teaching kitchens like these are part of the broader food-as-medicine movement that proponents say has the potential to improve health outcomes when it comes to preventing and treating disease. They can also help combat food insecurity, which one 2018 study showed contributed an additional $77.5 billion in health care expenditure in the U.S.
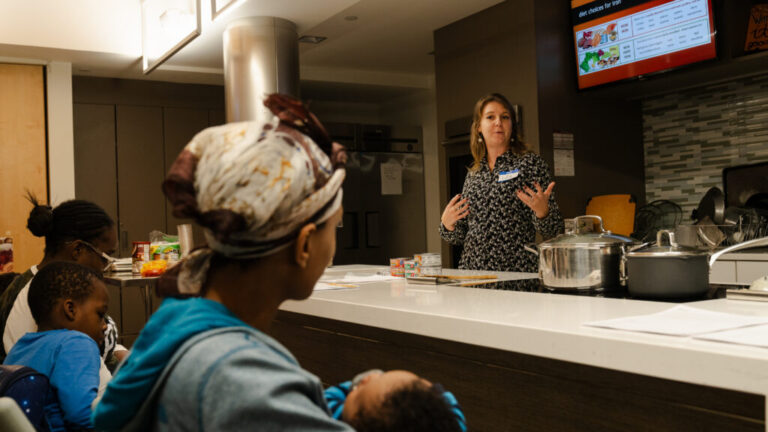
On this chilly December night, the topic was anemia in pregnancy, drawing a dozen adults and five children for instruction rather than hands-on cooking. Transportation to and from the class was provided for anyone who needed it.
The lessons, presented in both English and Spanish, note that rapidly growing bodies in childhood or in pregnancy need more iron than at other times. A PowerPoint on a screen above the ovens listed foods high in iron, like meat, fish, beans, eggs, and spinach, as well as foods that helped or hurt iron absorption, with berries and citrus in the former category and caffeine and dairy in the latter.
The staff prepared rice and beans for the group and offered blueberries, raspberries, and blackberries that the children scooped up at the end of class. Cooking eggs without cheese would be new for some families, but one woman offered onions and peppers as her choice.
One participant had a question about canned chicken — a product some attendees had never seen — versus organic fresh chicken. As GROW dietitian Lisa Burke had noted before the class began, canned meats are important for people who live in a shelter or lack access to a refrigerator. Her answer to the class member, acknowledging she couldn’t say one was better than the other, was that both are high in iron.
As the class concluded, families took home canned meat and fish, fruit, to-go containers of a Haitian-inspired dish of rice and beans, and gift cards to the grocery stores Stop & Shop and Market Basket. On the way out, they registered for the hospital’s food pantry, where participants’ anemia or other conditions would be noted so they would receive appropriate foods for two visits a month.
Anemia was not the only reason Peebles had attended that evening with her two sons. “We come to all of these,” she said. There’s a class on lactose- and dairy-free meal alternatives, and to her surprise, Egypt has lactose intolerance, unlike his brother, two sisters, and anyone else in the extended family.
“They focus on topics like cholesterol, blood pressure — all that’s healthy, which is perfect.”

How teaching kitchens work
The term “teaching kitchen” was coined by David M. Eisenberg, the director of culinary nutrition and adjunct associate professor of nutrition at the Harvard T. H. Chan School of Public Health. In 2006, he co-founded the Healthy Kitchens, Healthy Lives educational conference to bring together chefs and cooks with medical and public health experts. The goal was to test the theory that teaching kitchens could have a profound and measurable impact on patients’ behavior, clinical outcomes, and the cost of care.
At Boston Medical Center, the birth of this health-enhancing showroom was largely fueled by the existing food pantry. The food pantry was started in 2001 by Deborah Frank, the director of the Grow Clinic for Children at Boston Medical Center, after she noticed the direct health and social impacts of her patients who struggled with food insecurity. She was “tired of having mothers burst into tears when I tell them that their children have to eat three times a day,” Frank recalled.
Frank and her team partnered with the Greater Boston Food Bank to source fresh produce. Patients struggling with food insecurity are referred to the food pantry by BMC providers who write prescriptions for foods that best promote physical health, prevent future illness, and facilitate recovery.
But even though the food pantry facilitates access to fresh and healthy food, not everyone may know what to do with it. Frank recalls one day when the delivery included “huge squashes.”
“Our nutritionist handed one to a mother who looked at it as if she had just been given a basketball,” she said. Adopting a healthy diet long-term goes beyond just having the opportunity to access nutritious food — it requires knowledge on food preparation, storage, and more.
That’s when the idea of the teaching kitchen came into place. “How can we teach people how to use unfamiliar foods to make delicious, affordable, and sustainable meals?” said Frank. Eating healthily can be challenging with a tight budget and hectic schedule. The mission of the kitchen is to create an inclusive learning environment that strives to celebrate the diversity of food.
Each of the classes is designed to accommodate the realities of patients’ lives. “Our classes are built to address limited access and low resource kitchens,” said Olivia Weinstein, the director of nutrition innovation and implementation at Boston Medical Center, who leads the teaching kitchen initiative.
With her sister, Weinstein also created a free app called Pursuit, where families can find recipes to mix and match, customize existing recipes to include ingredients they might be more familiar with, and be exposed to a range of cooking techniques using appliances they might already have on hand.
The app is now used by hospitals across the country, including Boston Medical Center, as it can be customized to meet the needs of specific programs. At the GROW Clinic, the app is called Feeding My Family.
“We have a lot of families in shelters and a lot of families who don’t have consistent access to shelf-stable food,” Burke said. “So in all our in-person classes, the majority of the food can be found in the food pantry or through WIC benefits. So we’re using these ingredients, these recipes, in the teaching kitchen, then going through the clinical information. Then the families can then access what they did again on the app.”
Heidy Sulamita, a 21-year-old mother who attended the anemia class, said the classes are helping her while she experiences postpartum depression after the birth of her daughter. They’ve opened up her world to information about how nutrients are absorbed in the body, what foods are iron-rich, and how to cook healthier — all of which is helping improve the health of herself and her daughter.
“It was uplifting to be able to interact with people at Boston Medical Center and really join this community of Spanish-speaking moms who I could go to for advice,” she said. She migrated from Guatemala to flee sexual trafficking in the hope of a better life in the United States, and noted the classes have helped her make new friends who she can relate to.
Sulamita received the opportunity to join this community when the clinic reached out to her directly. GROW Clinic specifically targets pregnant women, mothers with a lot of children, and young mothers like her with the goal of improving health outcomes among this selected cohort.
Funding food as medicine programs
Food as medicine programs like the teaching kitchen can be expensive to operate. In the case of Boston Medical Center’s initiative, funding from private donors keeps the teaching kitchen running and makes classes available at no cost to patients, said Weinstein. However, one of their programs, called Diabetes Essentials, bills patients’ insurance, since many plans cover diabetes self-management education and training.
Grants are another way the BMC kitchen has been able to secure funding. Weinstein and her colleagues recently gained a grant to pursue a research study looking at how culinary education influences patients who are experiencing psychotic symptoms. This initiative is part of an overall collaboration with BMC’s Wellness and Recovery After Psychosis program, a wellness series that offers a variety of services for patients.
“We recently finished a pretty robust 12-week intervention with a two-arm study. When the research study ended, we collected that data, but then we turned the intervention into a once-a-month class because patients really enjoyed it,” Weinstein told STAT. She has also applied for both internal and external grants for programs on staff wellness, health education, and specific chronic conditions.
Amid growing interest in food as medicine initiatives across the nation, the Biden Administration has started to approve requests in certain states for Medicaid to cover nutrition interventions aimed at reducing health care costs.
However, there’s not a single definition of “food as medicine,” and Medicaid pilot programs vary from state to state. Some states’ coverage may include food prescriptions, food safety education, or cooking classes via teaching kitchens. Currently, the Centers for Medicare & Medicaid Services requires such programs to be neutral to the federal budget and capped at 3% of the state’s total Medicaid spend.

Reclaiming food sovereignty
A key part of the conversation in keeping teaching kitchens sustainable is sourcing the food itself. Purchasing food, especially fresh produce, for every class adds increased costs on top of kitchen operating expenses. The BMC teaching kitchen not only partners with the BMC Food Pantry, it grows fruits and vegetables on a rooftop farm to source produce for the classes.
However, the desired fruit or vegetable for a given recipe may not necessarily be in stock at the pantry or grown in season at the farm. Staff members make sure to have a range of fresh produce available during classes so patients can customize their meal with what they enjoy.
“Given how food systems are really complicated, we use recipe frameworks,” said Weinstein. During virtual sessions, patients are encouraged to use what they have on hand and what they want to use. The goal is to help patients put their own spin on the proposed meal in a way that is still nutritious, but culturally appropriate and enjoyable to them, said Weinstein.
“The goal is not to Westernize and medicalize our diet,” said Weinstein.
Another one of the program’s goals is to expand nutrition access and education beyond BMC’s premises. “We have good engagement with our programs, but we’re never at capacity,” said Weinstein. “And we’re finding that it’s because the hospital is kind of hard to get to and it’s not the most approachable environment.”
With this goal in mind, Boston Medical Center has provided a $1 million loan to help BIPOC-owned Nubian Markets — a grocery store, cafe, and community space located in Nubian Square — with the goal of helping to expand residents’ access to fresh, healthy foods and thus improve their social determinants of health.
The next step for BMC’s teaching kitchen staff is to bring cooking classes to Nubian Markets, meeting this predominantly Black community where they are as the hospital is often not accessible to them. The recipes, created by chef Ismail Samad of Nubian Markets, are inspired by cultures of the African diaspora. Nutrition and medical experts from BMC will collaborate with Chef Samad and his team to help guide the nutrition education behind these cooking classes in “support group” style.
“How can food as medicine programs sustainably support communities, rather than us as health care workers deciding those people who’ll benefit from it?” Weinstein asked.
Nutrition as medicine for the next generation
When Mallika Sabharwal was a first-year family medicine resident starting her training at BMC, one of her first bonding experiences onsite was at the teaching kitchen.
“During our orientation week, we had a session in the teaching kitchen and it served as an icebreaker where we played like Top Chef and split up among our colleagues to make a dish,” said Sabharwal, now a board-certified family medicine physician and preventative medicine fellow at BMC.
As a medical student, Sabharwal only had two hours of medical education on nutrition. However, working with the teaching kitchen as a resident and now as a fellow has broadened her knowledge on nutrition, food access, and overall cooking skills, she told STAT.
“Medical education should start thinking of nutrition as medicine and be equipped with resources to educate students with knowledge around nutrition and cooking so they can guide their future patients,” said Sabharwal. BMC aims to do just that with a six-week elective called Eat To Treat for Boston University Medical Students, which focuses on integrating nutrition and diet education through cooking and counseling techniques.
Led by Weinstein, medical students are taught cooking and meal preparation skills via hands-on interactive classes. At the end of the elective, students hold a cook-off competition in which they are asked to make meals appropriate for fictional patients who have different dietary restrictions and cooking equipment limitations.
“It was a fun way to learn nutrition in medical school ,and I even got to personally benefit from it,” said Lucia Ryll, who took the elective in 2018 when she was a first-year medical student. Now a first-year surgical resident in otolaryngology at BMC, she noted that the elective has inspired her to incorporate nutrition counseling with patients on her way to becoming a head and neck surgeon.
“One of the helpful things that I learned in the teaching kitchen was taking a 24-hour food history, where you would ask a person what they ate for breakfast, lunch and dinner” to get an idea of what their typical diet might look like, said Ryall. The exercise can also clue providers in about whether patients may be struggling with food insecurity.
Education from the teaching kitchen also spreads the message that the conversation around nutrition habits doesn’t always have to come from a primary care provider — specialists may have useful ideas, too. “Being able to suggest small changes, like, try watering down juice, as they get reiterated by different people like primary care and different providers, it might sink in a little bit more for patients,” said Ryll.
Sabharwal said she plans to adopt the teaching kitchen model wherever she lands up after her fellowship is over, continuing to offer healthy eating advice for a diverse array of patients. “Some are more interested in prevention, while others are totally new to nutrition and are like, what is protein?” she said. “I think there’s space for all of that.”